DISCLAIMER
This blog post details the possibilities of sleep paralysis in polyphasic sleep mostly during adaptation phase. There are explanations of how frequently it appears during the polyphasic schedules in the current system. There is no direct research that draw a perfectly conclusive correlation between these two sleep phenomena. Thus, any conjectures and reasonings in this blog post should be taken with a grain of salt. More research is necessary in this area.
Introduction
Experiencing sleep paralysis is not uncommon in our daily life. It may occur during our slumber from time to time. Encounters with sleep paralysis are usually unpleasant at best, and nightmarish at worst. Common descriptions of sleep paralysis include, but not limited to:
- Visualization of demonic or otherworldly physical beings in the bedroom, or even lying right next to the sleeper.
- Feeling paralysis in all four limbs
- The inability to utter any words
In this blog post, the focus is on isolated sleep paralysis, a type of paralysis that occurs right after sleep onset or awakening. These encounters are usually random; however, there has been some research on sleep that can give some insights into isolated sleep paralysis’ contributors. This may be helpful for polyphasic sleeping.
At face value, sleep paralysis may not be common in polyphasic adaptation. Human activities may not constitute its occurrences, either. Regardless, an average polyphasic sleeper will have a small chance, if any, to run into sleep paralysis during polyphasic adaptations.
Factors that may introduce sleep paralysis
REM wakes & interrupted sleep
Isolated sleep paralysis was observed using a method of interrupting the monophasic sleep pattern of healthy participants. Specifically, waking them up after SOREM and a couple minutes of REM sleep induced paralysis1.
- No NREM or SWS wakes induced sleep paralysis since there were no apparent signs that suggest otherwise2.
- The distribution of REM sleep and SOREM circadian-wise (naturally and not with artificial lighting control) also factors in sleep paralysis frequency.
- NREM/SWS dominates the first portion of the night (9 PM to midnight); REM dominates the second portion as the night progresses toward dawn. However, sleep paralysis incidents occurred as often as possible without any time cues1 and only around 4 AM with controlled lighting environment3.
- The speculation is that a more REM-abundant time frame in the day can help mitigate sleep paralysis’ occurrence, such as dawn. Here, REM density is higher and natural for the body to obtain.
The interrupted monophasic sleep method bears some resemblance to the schedule Zoidberg, a failed experiment.
- Sleep deprivation quickly accumulates in this model.
- Chopping sleep into ~20-minute naps makes the body fail to get enough REM and SWS.
- REM wakes built up within just 2-3 days according to the creator of the schedule, Dr. Zoid from the Discord community.
- He also experienced muscle discomfort that persisted throughout the duration of the experiment. However, there was no specification of whether that was actually sleep paralysis or purely sleep deprivation.
Regardless, the experience seems to line up with the methods in both aforementioned experiments. Muscle discomfort, in a vague way, may resemble sleep paralysis where there is struggle in controlling muscle movements.
Chaotic circadian rhythm (e.g, night shift)
Among night shift nurses, only 12% of the subjects3 reported to experience some higher degree of paralysis especially when dawn approaches. Additionally, they also find it more difficult to stay awake at night and experience cognitive impairment during nighttime. The difference is that sleep paralysis incidents focus around morning (dawn/the start of the day) rather than all across the board like in the 2002 study.
This is reasonable because of the pre-establishment that REM periods result in sleep paralysis; these REM periods are also abundant around morning time. Specific data for the “REM-peak hours” include:
- Lowest alertness level
- Body temperature at the minimum
- Low levels of physiological and biological functions around 4 AM.
Circadian-wise, these details match the body’s need to rest and the necessity to be in deeper stages of sleep for recovery. This is because they are sleep-inducing cues. The resistance to resting (which is very important why we sleep at night) causes the deterioration of sleep quality. This results in several impairments in bodily functions that night shift workers have. They often show higher cardiovascular risks and other chronic diseases.
Tolerance & sensitivity to changes in sleep patterns
This is an individual factor and varies from case to case1. The general pointer is that people who have experienced sleep paralysis have lower tolerance to changes in sleep patterns. This is conjecture material, so it requires more data for further conclusions.
- Theoretically speaking, those who do not have trouble going back to sleep after an interrupted wake tend to have better overall sleep quality. This is because they are able to continue their sleep quickly and maintain sufficient sleep duration.
- On the other hand, those who cannot go back to sleep after being woken by stimuli tend to have lighter sleep. They may also be susceptible to insomnia. This is stress as a result of lost and interrupted sleep and more intermittent wakes.
- The lack of “flexibility” indicated in this article supports this perspective. Flexibility in this context refers to the ability to adapt to different sleep environments. This remains a very indirect correlation and needs further findings to confirm.
Sleep deprivation or REM deprivation
Back to the night shift nurse study, signs of sleep deprivation were clearly documented. This includes the struggle to stay awake and high levels of sleepiness just like in polyphasic sleep adaptation. This leads to the lack of REM sleep, and possibly some SWS as well. An interesting observation from the study is that partial sleep deprivation is a result of night shift work; it reduced daytime sleep of the nurses. Consequently, it is possible to hypothesize that REM sleep deprivation in general may be related to sleep paralysis.
There was no specification of whether any of the nurses were practicing or had practiced any sleep pattern other than monophasic sleep; however, it is possible they were monophasic and had to reduce their monophasic core duration due to their occupation. Polyphasic sleeping simply did not fit their work schedule while requiring consistency during adaptation to make it work.
It is also reasonable to assume that their sleep started after the night shift, which is anywhere from 8 to 10 AM. The outcome is the late wake into noon or early afternoon, and feeling of listlessness.
- Circadian-wise, this REM peak region leads to lower amount of SWS in the core; at one point the core sleep has to extend to resolve SWS deprivation while also covering necessary REM amounts.
- Granted the nurses are busy with daily commitments, their core sleep may not be as consistently long as that of a normal monophasic duration of 7-9h.
- Reducing the core length cuts into REM sleep. Together with some lacking SWS, this leads to partial and potentially chronic sleep deprivation.
- The nurses reported paralysis incidents to occur BEFORE their sleep. This implies that under considerable sleep pressure and sleep deprivation, sleep paralysis can occur.
Other determinants
There is no clear evidence for these factors on sleep paralysis2. Other factors such as mental disorders, substance abuse, etc. are also possible. More research in this field would be helpful.
However, narcolepsy, which is part of genetic factor, is a suspect in developing sleep paralysis2. None of the subjects were having narcoleptic symptoms, but this does not exclude the chance that they might have it in the future.
Data and findings demonstrate that they do not exhibit the same SOREM and REM periods as in narcoleptic patients; however, they did exhibit certain elements similar to those in narcoleptic patients. For example, there are physical manifestations of sleep paralysis such as:
- Inability to speak
- Hallucinations
- Irritation
- Some kind of emotional swings such as fear
These signs are common in narcoleptic individuals.
Current anecdotal observations, reports and concerns in the polyphasic sleep
In the Discord and Reddit polyphasic community, there are very few reports on sleep paralysis.
- From personal accounts and experience, there are only a couple cases of adaptation to more extreme schedules such as Bimaxion and Everyman 3. However, there are no reports from successful adaptations.
- Milder schedules such as Biphasic, Everyman 2, Dual Core 1 contain no reports.
- The number is not comprehensive, due to the inconsistent amount of logs and personal preference of whether to report it or not.
- With such a small sample size, however, intense sleep deprivation and REM wakes may seem to play some role in creating sleep paralysis.
- Other factors such as diet, lifestyle, personal hygiene might or might not develop more frequent encounters with sleep paralysis. Nevertheless, there were no reports on this end from polyphasic sleepers.
Tips
Furthermore, concerns with sleep paralysis do potentially spike during scheduling. Given that a research article on night shift nurses sparked some insights into sleep paralysis by a messy circadian rhythm, consider these carefully when scheduling a polyphasic sleep pattern.
- The favorable choice would be to focus on sleeping at night, or getting as much night sleep as possible. This would cover some or most of the graveyard hours (midnight to 8 AM).
- An even safer approach is to sleep at consistent times everyday or have some flexibility within a small sleep window. The consistency will assist with a more stable circadian rhythm.
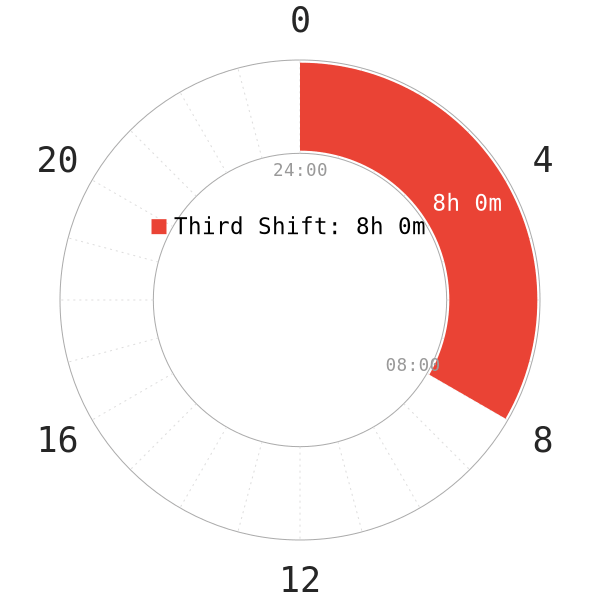
- Thus, third shift workers or any polyphasic schedules with no sleep within the graveyard hours will likely come across sleep paralysis more often. This includes increasing fatigue, harder adaptations and prolonged sleep deprivation as well.
- It is also wise to stop adapting to a schedule if oversleeps keep happening. Recover from all sleep debt before more bad wakes (REM/SWS wakes) occur.
All in all, a reasonable sleep pattern along with healthy life choices may lead to blissful sleep and shield sleepers from unpleasant events like sleep paralysis.
Main author: GeneralNguyen
Page last updated: 2 April 2021
Reference
- Takeuchi, T., Fukuda, K., Sasaki, Y., Inugami, M., & Murphy, T. I. (2002). Factors Related to the Occurrence of Isolated Sleep Paralysis Elicited During a Multi-Phasic Sleep-Wake Schedule. Sleep, 25(1), 89–96. doi:10.1093/sleep/25.1.89. [PubMed]
- Takeuchi, T., Miyasita, A., Sasaki, Y., Inugami, M., & Fukuda, K. (1992). Isolated Sleep Paralysis Elicited by Sleep Interruption. Sleep, 15(3), 217–225. doi:10.1093/sleep/15.3.217. [PubMed]
- Folkard, S., Condon, R., & Herbert, M. (1984). Night shift paralysis. Experientia, 40(5), 510–512. doi:10.1007/bf01952412. [PubMed]
