Introduction
Sleep tracking remains a relatively new science, especially in polyphasic sleeping. In order to accurately track sleep stages, you would need to monitor brain waves. The most common tool for this purpose is an electroencephalogram (EEG), which records electrical activity of the brain. Several different commercial devices exist, each with difference in prices and accuracy. The purposes of this section are to:
- Describe the necessity of using EEGs
- Which EEG devices the community recommends, and
- How to make an EEG at home.
Content
- Wrist-worn Sleep Trackers
- Phone Apps
- Tracking Sleep Without Machines
- Electroencephalography
- Actigraphy and Accelerometry
- Electrooculography
- Electrocardiography
- Polysomnography
Review of Commercially Available Sleep Trackers
There are many different sleep trackers on the market. However, several of them have very poor accuracy (See below). This section will provide you with the community recommendations so that you know what to purchase. Most commercially available devices only report the total amount of sleep but NOT the specific sleep stages (NREM1, NREM2, SWS, REM). When they do report those sleep stages, they often limit them to a subset, like “light sleep” and “deep sleep”.
Some of these products have very little independent research to back up their accuracy claims. We have made comparisons with scientifically supported accurate EEG devices within the community while no accuracy research is available. The accuracy rate in these sections refer to the accuracy of determining specific sleep stages.
Wrist-worn Sleep Trackers
(Jawbone UP, Mi band, Fitbit, Galaxy watch etc.)
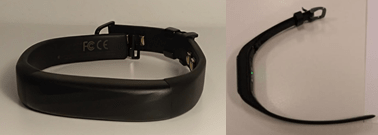
| Price | $30-200 |
| Accuracy | < 50% |
| Community tested | Yes |
| Conclusion | Not recommended |
| Comment | Some are good at determining the moment you fall asleep, but they are very inaccurate at specifying sleep stages. |
Phone Application
| Price | $10 |
| Accuracy | < 50% |
| Community tested | Yes |
| Conclusion | Not recommended |
| Comment | Very bad at giving accurate data. |
Oura Ring

Image link: https://ouraring.com/products/
| Price | $360 |
| Accuracy | 50 – 60%1 |
| Community tested | Yes |
| Conclusion | Not recommended |
| Comment | The study on the accuracy of the ring categorized NREM2 and NREM3 in the same category; thus, this artificially inflates its supposed accuracy. Testing in the community confirmed that the ring gave very inaccurate data. The Oura ring 2 and 1 have the same accuracy. |
Zeo

| Price | $40 – 100 (second hand) |
| Accuracy | 75%2 – 81% |
| Community tested | Yes |
| Conclusion | Highly recommended |
| Comment | The only way to get your hand on a Zeo has been through second-hand sellers ever since the company went bankrupt in 2013. However, it is still a very good choice for tracking your sleep. More information of this product is available in the Zeo page. |
Olimex OpenEEG

| Price | $200 |
| Accuracy | Up to 83 % mean accuracy3 |
| Community tested | Yes |
| Conclusion | Highly recommended |
| Comment | A semi DIY-solution. It can be a bit of a hassle to set up, but once finished, the accuracy of the device can be very high. More information of this product is available in the Olimex page. |
Dreem

| Price | $500 |
| Accuracy | Unproven* |
| Community tested | Yes |
| Conclusion | Recommended |
| Comment | The graphs are very hard to read, and the accuracy is questionable. Nonetheless, if you have enough money and are unable to find another EEG, then it could be a fair solution. |
*A study on the Dreem website determined the accuracy of the tracker based their whole conclusion on how accurately it tracked SWS. They also assumed the accuracy regarding the other sleep types, completely disregarding actually measuring light sleep and REM sleep4. It is, therefore, possible that it tracks SWS well and the other sleep stages very poorly.
Neuroon

Image link: https://www.indiegogo.com/projects/neuroon-open-world-s-smartest-sleep-tracker#/
| Price | $200 |
| Accuracy | 23% |
| Community tested | No |
| Conclusion | Not recommended |
| Comment | While the community has not tested the product, it does not have good Amazon reviews. It has poor accuracy, hard to get a good signal from it. It also has bad battery life, etc. |
The company lied about the device being the first EEG in the world that uses advanced sleep staging. However, there was no scientific article that would describe its accuracy. Thus, it should be somewhat telling why people dislike this product.
“Neuroon is the first device on the consumer market that measures EEG (brainwaves) and uses this data for advanced sleep staging. Neuroon is equipped with 3 dry, golden-plated electrodes, pulse- oximeter sensor and accelerometer which are enough for getting comprehensive data about sleep.”
(excerpt of https://neuroonopen.com/#, posted 4.3.2019, accessed 30.1.2019)
The Neuroon was worse at determining total sleep time, wake after sleep onset, the number of awakenings, sleep onset latency, and sleep efficiency than the Fitbit5. In addition, it was also bad at accurately labeling sleep stages (LNREM 5%, SWS 50%, REM 5%)6, resulting in an average accuracy of 23%.
Tracking Sleep Without Machines
While it might not be nearly as accurate to sense what sleep stages go into naps or cores as with an EEG, certain sleep stages typically leave some ques. Sensing what percentage of specific sleep stages a core has is not likely, but it is often possible to determine the sleep stage at awakening. This is especially important for naps. Because they are so short, their structure will usually follow this pattern:
Wake – NREM1 – NREM2 – (REM – NREM2 -) SWS
- You should avoid SWS wakes at all cost, because that sleep stage is usually difficult to wake from.
- Whether the nap has REM sleep or not highly depends on the time of the day, as well as sleep pressure.
- As adaptations progress, you can expect the pattern of sleep stage as presented above. This starts with being awake during naps, then NREM1, NREM2 and finally, hopefully REM sleep.
- If naps are very late during the day, the REM – NREM2- block could be skipped over, resulting in an SWS wake. This is unwanted and you should consider taking naps earlier if this happens regularly.
Here is a list of features to look out for to determine what the last sleep stage was.
NREM1
- Hypnic jerks (muscle contractions)
- Reduced awareness of surroundings
- Auditory and visual hallucinations
NREM2
- Time jumps (feeling like no time has passed)
SWS
- Disorientation
- Grogginess
- Sleep walking
- Difficulty waking up
REM
- Erections7
- Vivid dreams (around 80% of all dreams happen during REM sleep8)
- Time dilation
- Disorientation
Temporal Units
Dreams can occur in all sleep stages, but mostly in REM sleep. Thus, it is inconclusive how much REM sleep was present just because the nap contained a dream. An approach to determining your sleep stage is dream recall and evaluation. This method is particularly useful to determine if a nap had only NREM or also REM.
The article “Slow Wave Sleep Dreaming”, by Cavallero, Corrado et. al. published in November 19929 mentioned this method. Multiple other dreaming articles also reference this article.
You can determine which sleep stage the dreaming occurred in with reasonable accuracy by counting the amount of temporal units (TU) in the dream. For REM sleep, the average was 5.10 ±4.14 TU, while only 1.88 ±1.68 TU for SWS. This means that dreams that have 4 or more TU’s are likely from REM sleep, while dreams of 1-2TU are more likely SWS. However, the article mention similar complexity for the other NREM stages, but don’t give concrete numbers.
Definition & Use
To cite the paper directly:
“A temporal unit was defined as “consisting of whatever activities
could have occurred synchronously and were not described by the
subject as having occurred successively. Judges were told to assign
a new temporal unit whenever(a) a character performed an activity
that could not, in waking life, be synchronous with her/his previous
activity(b) a character responded to another character or event; or
(c) there was a topical change in vaguely recalled conversation”
Therefore, to clarify this with an example, consider the following scenario in a dream:
You are talking to someone about cars and that person is doing the dishes. After a while, you are talking about dogs and then going to the supermarket. The dream stops before you arrive.
That dream would be 3 TUs:
- A character is responding to you, while someone else is doing an activity. Because these happen at the same time, that is still 1 TU.
- The topic of the conversation changed.
- A character is doing something that could not be synchronous with what you did before.
If you are unsure what to make out of a dream, you can consult the #dreaming channel on the Discord. For more background information on this method, refer to the scientific paper, as it is only 5 pages long.
Electroencephalography
Electroencephalography (EEG) is a sleep tracking method for monitoring the electrical activity of the brain. EEGs are what the polyphasic community recommend for people interested in sleep tracking, as they are the most reliable single-method. Depending on the sleep stage classification program, the accuracy of single-channel EEGs can reach from around 70%10 to as high as over 90% when compared to polysomnograms (PSGs)11.
EEGs can be very expensive, but some devices are cheaper than others. Further sections will contain information about specific EEGs.
Actigraphy and Accelerometry
Actigraphy refers to tracking sleep with motion sensors. However, many commercially available wrist worn sleep trackers and phone applications use accelerometers instead, which detect acceleration instead of motion. This section will cover both of these sensor types because of the similarities within the sensors.
- Sleep tracking with only an accelerometer and/or a microphone from phone applications show poor accuracy in sleep phase detection12.
- Wristband trackers (Bodymedia, Fitbit) show poor wake detection accuracy.
- SleepTracker, Jawbone UP, and Basis Band have no research public to verify their accuracy, but they work with the same instruments as other wrist worn trackers. Thus, it is safe to conclude that they will also have a poor accuracy13.
- The Fitbit and Jawbone overestimate their total sleep time and sleep efficiency and underestimate wake after sleep onset comparing metrics from polysomnography14.
- Most devices show similar accuracy when they were based on the same type of sensors (accelerometer, noise) or device types (phone, wristband, etc.) This means that the accuracy of most wrist worn devices is questionable.
- Studies that have specifically analyzed the accuracy of actimeters have concluded that the sleep stage determination accuracy is very poor, with only less than 50%15 and 55%16.
- Many studies determining the accuracy of actimeters have also relied on inappropriate statistical techniques, specifically correlations and comparison of means to determine the validity of actimeters17.
- However, clinically available actimeters (not to be confused with commercially available cheap alternatives) are very accurate at determining total sleep times18,19. Clinically available actimeters cost a lot and should therefore not be favored over tracking brainwaves.
Electrooculography
Electrooculography (EOG) refers to the sleep tracking method of monitoring eye movements with sensors. Because the eye is a bit magnetic, its movements are trackable, which facilitates distinguishing when people are in NREM and REM sleep20.
EOGs are able to distinguish between rapid eye and non-rapid eye movements with a very high accuracy (82%)21.
Electrocardiography
Electrocardiography (ECG) is based on tracking the heart rate with electrical impulses. This can then be used, usually in combination with respiratory inductance plethysmography (RIP)22 or as a component in polysomnography. ECGs often use around 12 electrodes to track the heart rate of people.
The accuracy of only ECGs in determining sleep stages was 41%23 and 69% with the aid of RIP22. Therefore, simply using ECGs to determine sleep stages will not yield favorable results.
Polysomnography
Polysomnograms (PSGs) monitors many bodily functions, including brain activity (EEG), eye movements (EOG), muscle activity (EMG), and heart rhythm (ECG). PSGs are popular in the medical field to monitor sleep as accurately as possible. Because of this, they are often used as the baseline when comparing other tracking methods.
PSGs are very expensive; however, because most tracking methods use electrodes, it might be possible for people to simply place the electrodes to monitor specific movements or activities for a higher accuracy. At the same time, they can apply the right classification programs if they decide to build a PSG of their own.
Depending on the EEG, it might be possible to move the electrodes into such positions to monitor both brain activity and eye movements simultaneously to yield a higher accuracy. This procedure is very often done as the standard setup.
Main author: Crimson
Page last updated: 2 April 2021
Reference
- De Zambotti M, Rosas L, Colrain IM, Baker FC. The Sleep of the Ring: Comparison of the ŌURA Sleep Tracker Against Polysomnography. B. 2017;17(2):124-136. doi:10.1080/15402002.2017.1300587. [PubMed]
- SHAMBROOM JR, FÁBREGAS SE, JOHNSTONE J. Validation of an automated wireless system to monitor sleep in healthy adults. Journal of Sleep Research. 2011;21(2):221-230. doi:10.1111/j.1365-2869.2011.00944.x. [PubMed]
- Han J, Zhao Y, Sun H, et al. A Fast, Open EEG Classification Framework Based on Feature Compression and Channel Ranking. F. 2018;12. doi:10.3389/fnins.2018.00217. [PubMed]
- Debellemaniere E, Chambon S, Pinaud C, et al. Performance of an Ambulatory Dry-EEG Device for Auditory Closed-Loop Stimulation of Sleep Slow Oscillations in the Home Environment. F. 2018;12. doi:10.3389/fnhum.2018.00088. [PubMed]
- Liang Z, Nishimura T. Are wearable EEG devices more accurate than fitness wristbands for home sleep Tracking? Comparison of consumer sleep trackers with clinical devices. In: 2017 IEEE 6th Global Conference on Consumer Electronics (GCCE). IEEE; 2017. doi:10.1109/gcce.2017.8229188
- Liang Z, Chapa Martell MA. Validity of Consumer Activity Wristbands and Wearable EEG for Measuring Overall Sleep Parameters and Sleep Structure in Free-Living Conditions. J. 2018;2(1-2):152-178. doi:10.1007/s41666-018-0013-1
- Mann K, Pankok J, Connemann B, Röschke J. Temporal relationship between nocturnal erections and rapid eye movement episodes in healthy men. Neuropsychobiology. 2003;47(2):109-114. [PubMed]
- DEMENT W, KLEITMAN N. The relation of eye movements during sleep to dream activity: an objective method for the study of dreaming. J Exp Psychol. 1957;53(5):339-346. [PubMed]
- Cavallero C, Cicogna P, Natale V, Occhionero M, Zito A. Slow Wave Sleep Dreaming. Sleep. 1992;15(6):562-566. doi:10.1093/sleep/15.6.562. [PubMed]
- Foldvary N, Caruso A, Mascha E, et al. Identifying montages that best detect electrographic seizure activity during polysomnography. Sleep. 2000;23(2):221-229. [PubMed]
- Aboalayon K, Faezipour M, Almuhammadi W, Moslehpour S. Sleep Stage Classification Using EEG Signal Analysis: A Comprehensive Survey and New Investigation. E. 2016;18(9):272. doi:10.3390/e18090272.
- Policies and procedures of accreditation for programs in nursing education. No. 14-1437. NLN Publ. January 1972:1-21. [PubMed]
- Lee J, Finkelstein J. Consumer sleep tracking devices: a critical review. Stud Health Technol Inform. 2015;210:458-460. [PubMed]
- Froom J. Conversion to problem-oriented records in an established practice. A timed study. Ann Intern Med. 1973;78(2):254-257. [PubMed]
- Paquet J, Kawinska A, Carrier J. Wake detection capacity of actigraphy during sleep. Sleep. 2007;30(10):1362-1369. [PubMed]
- Jean-Louis G, von G, Zizi F, Spielman A, Hauri P, Taub H. The actigraphy data analysis software: I. A novel approach to scoring and interpreting sleep-wake activity. Percept Mot Skills. 1997;85(1):207-216. [PubMed]
- Baker M, Cohan R, Cooper C, Dunnick N. Dynamic, incremental computed tomography using a high heat capacity tube, solid-state detector, and automated injector. Potential in body imaging. Clin Imaging. 1989;13(3):189-194. [PubMed]
- Kroczek R, Mühlbauer W, Zimmermann I. Cloverleaf skull associated with Pfeiffer syndrome: pathology and management. Eur J Pediatr. 1986;145(5):442-445. [PubMed]
- Herscovici S, Pe’er A, Papyan S, Lavie P. Detecting REM sleep from the finger: an automatic REM sleep algorithm based on peripheral arterial tone (PAT) and actigraphy. P. 2006;28(2):129-140. doi:10.1088/0967-3334/28/2/002. [PubMed]
- Gopal I, Haddad G. Automatic detection of eye movements in REM sleep using the electrooculogram. Am J Physiol. 1981;241(3):R217-21. [PubMed]
- Bokhon N, Razumovskiĭ M, Mallabiu G. [Diadynamotherapy in the complex treatment of patients with herpetic keratitis]. Vestn Oftalmol. 1968;81(1):69-71. [PubMed]
- Fonseca P, Long X, Radha M, Haakma R, Aarts R, Rolink J. Sleep stage classification with ECG and respiratory effort. Physiol Meas. 2015;36(10):2027-2040. [PubMed]
- Scherz WD, Fritz D, Velicu OR, Seepold R, Madrid NM. Heart rate spectrum analysis for sleep quality detection. J. 2017;2017(1). doi:10.1186/s13639-017-0072-z.
