Introduction
Rapid-eye-movement (REM) sleep, or “paradoxical / dream sleep“, is an indispensable sleep stage in humans. Specifically, this sleep stage has had a long history since its discovery in 19531. Moreover, it is usually the last sleep stage in a normal human sleep cycle. The other 3 sleep stages are NREM1, NREM2 and slow-wave sleep.
In polyphasic sleeping, REM stage has always been the center of attention. This is largely attributable to its ability to generate very vivid dreams from short naps. Because there has been important, or even groundbreaking discoveries over the years, this post will only cover the most crucial points. Hopefully, as we get closer to fully understanding the behavior of this sleep stage, we can unravel more mechanics of polyphasic sleeping.
Characteristics of REM Sleep
Being a vital sleep stage, paradoxical sleep has a lot of unique characteristics on its own. The following descriptions may help determine its role on a polyphasic regime. This section will relay various mechanics of this sleep stage.
Vital Bodily Functions of REM stage
Over time, scientists have discovered the multiple roles that paradoxical sleep play in human well-being and ultimately, survival. Apparently, more functions of REM stage are still in the search, so this section will only deliver some of the most noteworthy functions of this sleep stage on humans.
Restorative Functions
- Memory consolidation and learning: Paradoxical sleep is known for its ability to consolidate procedural2 and emotional memories3. Both of these memories assist with learning different steps or procedural activities.
- Brain development: Newborns3 and growing individuals (e.g, teenagers) usually spend more time in REM. This is because brain functions are undergoing critical development stages.
- Sensorimotor development: Muscle atonia is a very typical trait of paradoxical sleep. Furthermore, growing bodies of evidence recently suggest that the sensorimotor system in humans can develop in REM stage. Certain brain regions also undergo REM twitches, such as the hippocampus and cerebellar cortex3.
- Mood regulation: Certain brain regions that are responsible for emotional responses are active during REM. These include: the amygdala, hippocampus and frontal cortex. Together with forming emotional memories, REM stage likely regulates mood changes4.
Other physiological functions of REM stage includes, but not limited to:
- Inhibiting thermoregulatory processes like sweating and panting to keep the body still during dreams5. However, this can lead to excessive sweating if one sleeps under thick covers. In another case a polyphasic schedule with a higher percentage of REM sleep may also result in sweating.
- On polyphasic schedules, REM-heavy naps allegedly feel like a long period of time has passed.
- Erections
Consequences of Inadequate REM
While there are many long-term consequences with REM deprivation, below we present some of the common ones.
- Mood disorder (e.g, anxiety, irritability)
- Reduced dream recall
- Impaired attention and executive functions5
- Increased mortality rate6
- Impaired learning abilities
- Increase pain sensitivity7
- Alter permeability of the blood-brain barrier by decreasing cerebral blood-flow8
How Much REM sleep to get daily?
- Similar to deep sleep, doctors and specialists often recommend ~90 minutes of daily REM for optimal performance. This value translates to ~20% of total sleep spent in REM alone9.
- As said earlier, teenagers or people with elevated REM requirements may require at least 120m of daily REM.
- On the contrary, REM stage creates the distinction between normal, long and short sleepers. Specifically, short sleepers need less REM daily to maximize their performance10.
NOTE: The recommended benchmark likely varies between individuals, but the concepts remain the same. One should aim for good amount of REM stage if it is currently below their functional baseline levels. Because mileage may vary, it is acceptable if a somewhat below the recommended REM baseline (e.g, ~70m REM daily) is natural and consistent for a long time. As an addition, this section will explore factors that can influence REM duration.
Factors that reduce REM sleep duration
Because there are unclear factors may remain controversial, we only list the most common ones with backed research.
- Alcohol11. While alcohol mostly delays REM latency, a sufficiently long sleep session will still cover all REM requirement. However, consuming alcohol before a REM-filled nap on a polyphasic schedule is heavily discouraged because of SWS induction.
- Hypoxia12. This condition disrupts REM stage and results in cumulative deficits.
- Most SSRIs13
- Very low-carb diets14
- Ramadan intermittent fasting15
- Age. The elderly get less REM as they age; however, they only witness steady decline of REM stage at very old ages.
Factors that increase REM sleep duration
Same as factors that reduce REM duration, only the most popular increasing factors are presented here.
- Melatonin16. However, it may affect SWS depending on individuals.
- Exposure to dim artificial light at night and during sleep17. This increase is a negative one, as it makes overall sleep shallower and inflates REM duration.
- Depression18. The study shows the disinhibition of REM stage duration, but mostly in the first sleep cycle, coupled with short REM latency. In addition, depression also boosts overall REM density.
- Age. Teenagers often spend more time in REM.
- Narcolepsy.
However, intensive learning periods increase REM density rather than duration19; this should not worry polyphasic sleepers who have to absorb a lot of academic materials.
EEG Characteristics
EEG features
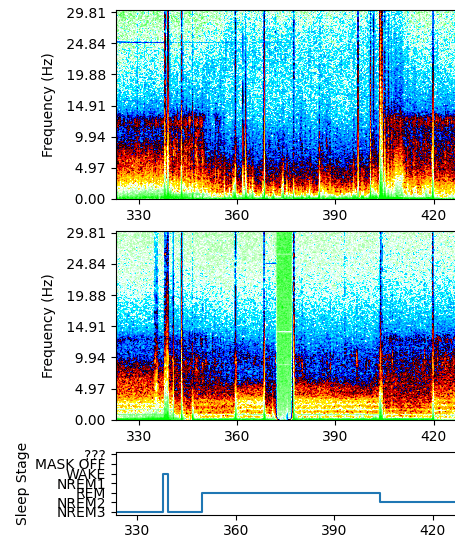
- The immediate EEG characteristics that set REM stage apart is the fast, low amplitude and desynched brainwaves that resemble the wake state20. Therefore, this is also a reason REM stage is called “paradoxical sleep”.
- Additionally, there is a 3-10 Hz theta rhythm in the hippocampus and 40-60 Hz in the cortex21. These values are also similar to those during normal wakefulness. Theta wave activity also dominates both of these brain regions during paradoxical sleep.
- The brain uses at least as much energy (in terms of glucose metabolism) as during wakefulness22. However, during NREM stages, energy expenditure is a lot lower.
- REM stage is responsible for ~80% of dreams23, most notably very vivid dreams. This is because of the increased activity of the forebrain, limbic and paralimbic regions24. Additionally, REM dreams also create phenomena such as lucid dreaming, sleep paralysis, and nightmares.
REM Density
Another unique feature of paradoxical sleep is REM density. REM density is defined as the number of eye movements per each 30-second epoch of REM stage25. It is also a defining feature of sleep satisfaction. Below are the details on REM density and how it works.
- From the name, during REM, human eyes move back and forth rapidly. However, this speed is still less than that during wakefulness.
- Under normal sleep condition, REM density tends to increase in the successive REM cycles, near the morning25. This observation seems to be in line with the circadian modulation of REM prevalence around morning hours. However, it is worth noting that REM density can receive a boost only when SWS pressure is low25.
- Under sleep deprivation condition, REM density decreases in the first night(s) of recovery/extended sleep25. However, the number of eye movements reach a stable level afterwards.
- Depending on the levels of REM density at awakening, sleep inertia can be moderate or intensified. It is likely that the higher the density of eye movements, the more groggy/dizzy it would feel to wake from REM.
Moreover, REM density is a different parameter from REM duration. Increasing the density does not necessarily increase the duration that a sleeper would spend in REM.
Conclusion
In sum, paradoxical sleep has very interesting yet underdeveloped features that make it a vital sleep stage. In specifics, REM stage is responsible for various critical biological processes to protect humans’ well-being and enhance their performance. The homeostatic and circadian regulations of paradoxical sleep are also largely different from its counterparts NREM sleep.
Main author: GeneralNguyen
Image by: Dakyne
Page last updated: 2 April 2021
Reference
- Foulkes, David. “Dream Research: 1953-1993.” Sleep 19.8 (1996): 609-624.
- FOGEL, S., SMITH, C., & COTE, K. (2007). Dissociable learning-dependent changes in REM and non-REM sleep in declarative and procedural memory systems. Behavioural Brain Research, 180(1), 48–61. doi:10.1016/j.bbr.2007.02.037. [PubMed]
- Peever, J., & Fuller, P. M. (2017). The Biology of REM Sleep. Current Biology, 27(22), R1237–R1248. doi:10.1016/j.cub.2017.10.026. [PubMed]
- Brown, R. E., Basheer, R., McKenna, J. T., Strecker, R. E., & McCarley, R. W. (2012). Control of Sleep and Wakefulness. Physiological Reviews, 92(3), 1087–1187. doi:10.1152/physrev.00032.2011. [PubMed]
- Institute of, Colten H, Altevogt B. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. January 2006. [PubMed]
- Leary, E. B., Watson, K. T., Ancoli-Israel, S., Redline, S., Yaffe, K., Ravelo, L. A., … Stone, K. L. (2020). Association of Rapid Eye Movement Sleep With Mortality in Middle-aged and Older Adults. JAMA Neurology. doi:10.1001/jamaneurol.2020.2108. [PubMed]
- Roehrs, Timothy, et al. “Sleep loss and REM sleep loss are hyperalgesic.” Sleep 29.2 (2006): 145-151. [PubMed]
- Gomez-Gonzalez, Beatriz, et al. “REM sleep loss and recovery regulates blood-brain barrier function.” Current neurovascular research 10.3 (2013): 197-207. [PubMed]
- Boulos, M. I., Jairam, T., Kendzerska, T., Im, J., Mekhael, A., & Murray, B. J. (2019). Normal polysomnography parameters in healthy adults: a systematic review and meta-analysis. The Lancet Respiratory Medicine. doi:10.1016/s2213-2600(19)30057-8.
- Hao, Y. L., Zhang, B., Jia, F. J., Li, X. L., Tang, Y., Ren, Y. Z., & Liu, W. H. (2014). A three-phase epidemiological study of short and long sleepers in a middle-aged Chinese population: prevalence and characteristics. Brazilian Journal of Medical and Biological Research, 47(2), 157–165. doi:10.1590/1414-431×20133430. [PubMed]
- Ebrahim, I. O., Shapiro, C. M., Williams, A. J., & Fenwick, P. B. (2013). Alcohol and Sleep I: Effects on Normal Sleep. Alcoholism: Clinical and Experimental Research, 37(4), 539`–549. doi:10.1111/acer.12006. [PubMed]
- Polotsky, Vsevolod Y., et al. “Intermittent hypoxia causes REM sleep deficits and decreases EEG delta power in NREM sleep in the C57BL/6J mouse.” Sleep medicine 7.1 (2006): 7-16. [PubMed]
- McCarthy, A., Wafford, K., Shanks, E., Ligocki, M., Edgar, D. M., & Dijk, D.-J. (2016). REM sleep homeostasis in the absence of REM sleep: Effects of antidepressants. Neuropharmacology, 108, 415–425. doi:10.1016/j.neuropharm.2016.04.047. [PubMed]
- Afaghi, A., O’Connor, H., & Chow, C. M. (2008). Acute effects of the very low carbohydrate diet on sleep indices. Nutritional Neuroscience, 11(4), 146–154. doi:10.1179/147683008×301540. [PubMed]
- Roky, R., Chapotot, F., Hakkou, F., Benchekroun, M. T., & Buguet, A. (2001). Sleep during Ramadan intermittent fasting. Journal of Sleep Research, 10(4), 319–327. doi:10.1046/j.1365-2869.2001.00269.x. [PubMed]
- Dijk, Derk-Jan, and Christian Cajochen. “Melatonin and the circadian regulation of sleep initiation, consolidation, structure, and the sleep EEG.” Journal of biological rhythms 12.6 (1997): 627-635. [PubMed]
- Cho, C.-H., Lee, H.-J., Yoon, H.-K., Kang, S.-G., Bok, K.-N., Jung, K.-Y., … Lee, E.-I. (2015). Exposure to dim artificial light at night increases REM sleep and awakenings in humans. Chronobiology International, 33(1), 117–123. doi:10.3109/07420528.2015.1108980. [PubMed]
- Armitage, R., & Hoffmann, R. F. (2001). Sleep EEG, depression and gender. Sleep Medicine Reviews, 5(3), 237–246. doi:10.1053/smrv.2000.0144. [PubMed]
- Smith, Carlyle, and Lorelei Lapp. “Increases in number of REMS and REM density in humans following an intensive learning period.” Sleep 14.4 (1991): 325-330. [PubMed]
- Steriade & McCarley (1990), “Brainstem Control of Wakefulness and Sleep”, §7.2–3 (pp. 206–208).
- J. Alan Hobson, Edward F. Pace-Scott, & Robert Stickgold (2000), “Dreaming and the brain: Toward a cognitive neuroscience of conscious states”, Behavioral and Brain Sciences 23. [PubMed]
- DEMENT W, KLEITMAN N. The relation of eye movements during sleep to dream activity: an objective method for the study of dreaming. J Exp Psychol. 1957;53(5):339-346. [PubMed]
- Luca Matarazzo, Ariane Foret, Laura Mascetti, Vincenzo Muto, Anahita Shaffii, & Pierre Maquet, “A systems-level approach to human REM sleep”; in Mallick et al, eds. (2011).
- Karamessinis, Laurie, et al. “Relationship between REM density, duty cycle, and obstructive sleep apnea in children.” Sleep 30.7 (2007): 837-843. [PubMed]
- KHALSA, S. B. S., CONROY, D. A., DUFFY, J. F., CZEISLER, C. A., & DIJK, D.-J. (2002). Sleep- and circadian-dependent modulation of REM density. Journal of Sleep Research, 11(1), 53–59. doi:10.1046/j.1365-2869.2002.00276.x. [PubMed]
