Introduction
There are a lot of biological rhythms in humans. This article will describe them in detail, mostly in the context of polyphasic sleeping. It is critical to have a healthy relationship to most, if not all these biological rhythms. However, while certain rhythms do not have to be very rigid, they can still have hidden effects on a polyphasic schedule.
Circadian Rhythm
The circadian rhythm is also sometimes referred to as the body clock. Additionally, it is a 24-hour rhythm that aligns with the local sunrise and sunset times. The most common alignments are primarily by light exposure1, breakfast2–5 and other factors.
Overall, the circadian rhythm consists of hormonal balances that fluctuate throughout the day to optimize bodily processes. Most notably, these include the regulation of melatonin6, which is important for SWS. Furthermore, it also affects the timing for the most efficient REM sleep.
- First, melatonin levels rise at dusk, signaling that sleep should begin.
- Second, because of the high melatonin levels, the first two sleep cycles contain most of the necessary SWS, and less REM than later sleep cycles.
- Lastly, the highest REM percentage in sleep is highest generally between 06:00 and 09:007.
Nonetheless, the following external cues can influence the circadian rhythm:
- Light between the frequencies 400 nm and 530 nm8 (blue and green light; from the sun or artificial light sources),
- Food, temperature9
- Exercise10
Nowadays, most people delay their circadian rhythm by evening screen time and artificial light exposure. Thus, all of these impede the proper accumulation of melatonin and can lead to sleep issues. However, filtering the light, and/or restricting the use of electronics within the two hours before bed can negate these issues. Additionally, purposely moving the circadian to sleep later is also possible, but you should be very careful. Your circadian is an important and complex hormonal regulatory system.
For more information on the effects of not filtering light and moving your circadian rhythm, visit Dark Period Course.
Homeostatic Process
The circadian rhythm and sleep-wake homeostatic process are two major processes that regulate sleep and alertness. While the circadian is fixed with a daily cycle, homeostatic refers to sleep pressure that builds over time. However, homeostatic pressure only reduces when you sleep. REM sleep and non-REM sleep have separate homeostatic pressures. The purpose of any homeostatic process is to maintain equilibrium to optimize daily body functions.
The higher the homeostatic pressure, i.e. sleep deprivation, the more it will override the circadian pressure at that time. Furthermore, the more sleep deprived you are, the more resistant your brain will be to changing your circadian rhythm11; this is important when attempting a standard schedule that is out of the SWS peak. You will want to set your new circadian rhythm by first using light and other cues. Still, this can take 1-2 weeks before your homeostatic sleep debt gets too high.
Polyphasic adaptation
- In a healthy, adapted brain, the homeostatic pressure only builds over the course of a day before being reset. The pressure also only raises just over a few hours in advanced polyphasic schedules.
- However, polyphasic schedules with naps relieve homeostatic pressure more frequently than once per day; specifically, naps can relieve REM pressure by containing 10-15 minutes of REM sleep.
- Light sleep naps also help alleviate the overall sleep pressure.
- On extreme schedules like Uberman, naps are supposed to contain SWS to frequently reduce SWS homeostatic pressure as well.
During polyphasic sleep adaptation, homeostatic pressures can vary rapidly because the brain has not yet adapted to the new sleeping pattern. Instead of returning to equilibrium every day, homeostatic pressures can build up over the course of several weeks. This is why adaptation to the vast majority of schedules is most difficult around week 3.
People entering a polyphasic schedule with pre-existing sleep debt (i.e. sleep deprivation) will experience intense homeostatic pressure sooner. This explains why polyphasic adaptation is challenging with a sleep deprived start. The difficulty is also proportional to the numbers of reduced daily sleep hours. In addition, adapting to new circadian entrainment (e.g. shifted schedules) is also a massive challenge. This is because it can feel like a jet lag.
Ultradian Rhythm
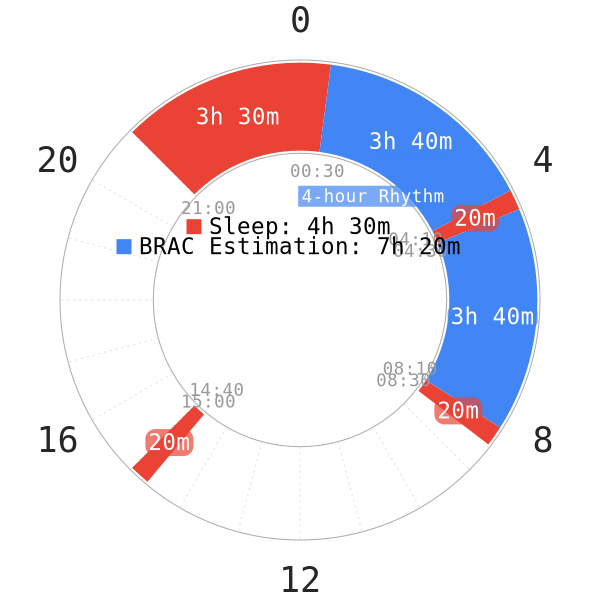
The ultradian rhythm is also sometimes known as BRAC, Basic Rest-Activity Cycle. This rhythm is a lot shorter than the circadian rhythm, and repeats itself roughly every 80-120 minutes12–14.
- BRAC’s are cyclical in manner: the brain starts alert and slows down for the second half. The last 20-ish minutes the brain is tired and slow.
- After this, the brain regains focus and the process repeats. Sleep cycles are possibly a manifestation of an ultradian rhythm during sleep.
- BRACs seem to consist of a multitude of different ultradian rhythms14. However, the alertness rhythms seem to be the most important for polyphasic sleepers.
Although not the most important factor, it can be a good idea to consider BRAC in scheduling. Specifically, this is usually the timing and placement of naps at the end of a BRAC. The Everyman 3 example above roughly demonstrates the concept of 2 BRAC cycles in scheduling. Almost 4 hours are awake hours, while the last 20 minutes is for resting.
Infradian rhythm
An infradian rhythm refers to a bodily rhythm with a frequency of less than one cycle every 28 hours. Some of the rhythms in this article are not actually bodily rhythms, but rather environmental. However, it is necessary to address them because of the cyclical nature of the rhythms and the similarity in effects. Examples of infradian rhythms are:
- Female menstrual cycle
- Seasonal cycle, which affects mood and sleep. The seasonal cycle in particular is interesting to polyphasic sleepers.
During winter, people need more sleep than during summer15.
- It seems like there is some elevation in REM during winter.
- There is also a shift in the circadian rhythm. All of this can decrease SWS. This results in a temporary state of hypersomnia16.
- People suffering from seasonal affective disorder during the winter also seem to have a lower tolerance for homeostatic pressure. As a result, they will need to sleep more frequently than others17.
For polyphasic sleepers, it might be beneficial to avoid starting adaptations during winter. There can be some increase in sleep needs, which boosts adaptation difficulty. However, due to the increased frequency of sleep episodes on polyphasic sleep, it might be beneficial to be adapted when winter arrives. This is because of the lowered homeostatic pressure that some people experience.
Additionally, the lunar phase cycle may be interesting to polyphasic sleepers and how it affects humans.
- It seems like when a full moon is nearing the amount of SWS decreases18
- Total sleep time decreases and sleep onset latency increases a bit19.
- The amount of REM sleep also seems affected depending on people’s gender.
- Women’s REM decreased
- Men’s REM increased close to a full moon18.
- There may also be more tiredness upon awakening when a full moon is near20.
However, whether sleep latency decreases and sleep quality would change in polyphasic sleepers is yet to be tested. Regardless, it may be sound to pay extra attention to alarm setup when a full moon is near. The increased levels of tiredness after waking up may also lead to involuntary oversleeps.
Main author: Jelte1234
Scientific sources: Crimson
Page last updated: 2 April 2021
Reference
- Pikulev A, Zyrianova T, Lavrova V, Khripchenko I. [Aspartate aminotransferase and glutamate dehydrogenase activity in the rat brain during infrared laser exposure]. Radiobiologiia. 1989;29(2):274-276. [PubMed]
- Lorenz K. The enmity between generations and its probable ethological causes. Stud Gen (Berl). 1970;23(10):963-997. [PubMed]
- Salgado-Delgado R, Angeles-Castellanos M, Saderi N, Buijs RM, Escobar C. Food Intake during the Normal Activity Phase Prevents Obesity and Circadian Desynchrony in a Rat Model of Night Work. E. 2010;151(3):1019-1029. doi:10.1210/en.2009-0864
- Morimoto Y, Arisue K, Yamamura Y. Relationship between Circadian Rhythm of Food Intake and that of Plasma Corticosterone and Effect of Food Restriction on Circadian Adrenocortical Rhythm in the Rat. N. 1977;23(4):212-222. doi:10.1159/000122669
- Longo VD, Panda S. Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan. C. 2016;23(6):1048-1059. doi:10.1016/j.cmet.2016.06.001
- Cajochen C, Kräuchi K, Wirz-Justice A. Role of melatonin in the regulation of human circadian rhythms and sleep. J Neuroendocrinol. 2003;15(4):432-437. [PubMed]
- Czeisler C, Zimmerman J, Ronda J, Moore-Ede M, Weitzman E. Timing of REM sleep is coupled to the circadian rhythm of body temperature in man. Sleep. 1980;2(3):329-346. [PubMed]
- Wright H, Lack L. Effect of light wavelength on suppression and phase delay of the melatonin rhythm. Chronobiol Int. 2001;18(5):801-808. [PubMed]
- Roepe P, Ahl P, Das G, Herzfeld J, Rothschild K. Tyrosine and carboxyl protonation changes in the bacteriorhodopsin photocycle. 1. M412 and L550 intermediates. Biochemistry. 1987;26(21):6696-6707. [PubMed]
- YAMANAKA Y, HONMA K, HASHIMOTO S, TAKASU N, MIYAZAKI T, HONMA S. Effects of physical exercise on human circadian rhythms. S. 2006;4(3):199-206. doi:10.1111/j.1479-8425.2006.00234.x
- Deboer T. Sleep homeostasis and the circadian clock: Do the circadian pacemaker and the sleep homeostat influence each other’s functioning? N. 2018;5:68-77. doi:10.1016/j.nbscr.2018.02.003
- Ootsuka Y, de Menezes RC, Zaretsky DV, et al. Brown adipose tissue thermogenesis heats brain and body as part of the brain-coordinated ultradian basic rest-activity cycle. N. 2009;164(2):849-861. doi:10.1016/j.neuroscience.2009.08.013
- Armitage R, Hoffmann R, Moffitt A. Interhemispheric EEG activity in sleep and wakefulness: Individual differences in the basic rest–activity cycle (BRAC). American Psychological Association. http://psycnet.apa.org/record/1992-98326-001. Published 1992. Accessed November 4, 2018.
- Kleitman N. Basic Rest-Activity Cycle—22 Years Later. Sleep. 1982;5(4):311-317. doi:10.1093/sleep/5.4.311
- Kume Y, Makabe S, Singha-Dong N, Vajamun P, Apikomonkon H, Griffiths J. Seasonal effects on the sleep–wake cycle, the rest–activity rhythm and quality of life for Japanese and Thai older people. C. 2017;34(10):1377-1387. doi:10.1080/07420528.2017.1372468
- Palchikov VE, Zolotarev DY, Danilenko KV, Putilov AA. Effects of the Seasons and of Bright Light Administered at Different Times of Day on Sleep EEG and Mood in Patients with Seasonal Affective Disorder. B. 1997;28(2):166-184. doi:10.1076/brhm.28.2.166.12994
- Cajochen C, Brunner DP, Kräuchi K, Graw P, Wirz-Justice A. EEG and subjective sleepiness during extended wakefulness in seasonal affective disorder: circadian and homeostatic influences. B. 2000;47(7):610-617. doi:10.1016/s0006-3223(99)00242-5
- Della Monica C, Atzori G, Dijk D-J. Effects of lunar phase on sleep in men and women in Surrey. J. 2015;24(6):687-694. doi:10.1111/jsr.12312
- Cajochen C, Altanay-Ekici S, Münch M, Frey S, Knoblauch V, Wirz-Justice A. Evidence that the Lunar Cycle Influences Human Sleep. C. 2013;23(15):1485-1488. doi:10.1016/j.cub.2013.06.029
- ROOSLI M, JUNI P, BRAUN-FAHRLANDER C, BRINKHOF MWG, LOW N, EGGER M. Sleepless night, the moon is bright: longitudinal study of lunar phase and sleep. J. 2006;15(2):149-153. doi:10.1111/j.1365-2869.2006.00520.x
